Micronutrient therapy
|
Definition |
|
Coronary heart disease (CHD) is an atherosclerotic and inflammatory disease of the heart, which manifests itself according to Álvarez-Álvarez et al. as stable angina, unstable angina, myocardial infarction or sudden cardiac death, and is one of the leading causes of death worldwide. To understand the different aspects of this disease, several consortia, case-control studies, epidemiological studies and genome-wide association analyses (GWAS) have been carried out. According to various studies, some risk factors associated with this disease include obesity, hypertension, hyperlipidemia, diabetes mellitus and homocystinuria, but factors such as stress and smoking may also play a significant role in CHD. In addition to these risk factors, there is another important factor, namely lifestyle, which plays a role in the development of cardiovascular diseases. In general, studies suggest, that a healthy lifestyle, an understanding of the above risk factors associated with CHD and early diagnosis not only contribute significantly to the improvement, but more specifically to the prognosis of patients with CHD. |
| Causes and symptoms |
|
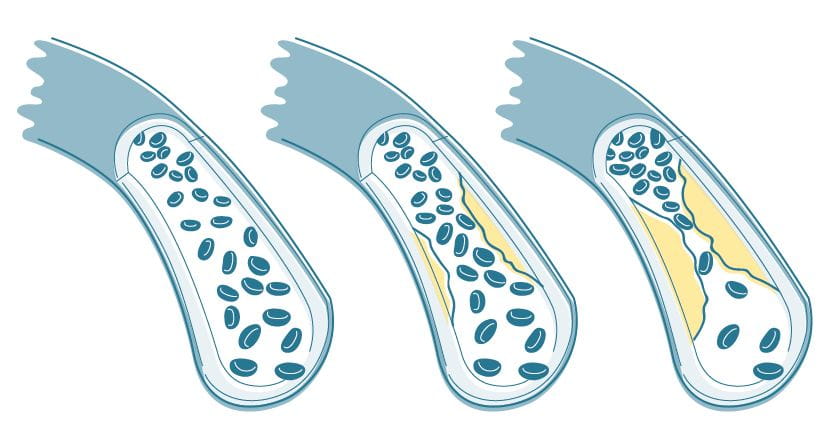
CHD is a cardiovascular disease caused by atherosclerosis or atherosclerotic blockage of the coronary arteries. Arterosclerosis is triggered when the endothelial function of the arterial wall is distrubed and the lipoportein droplets accumulate in the intima of the coronary vessels. Water-insoluble lipids circulate in the bloodstream by adhering themselves to apoliporoteins, which are water-soluble lipoproteins. In high concentrations, low-density lipoproteins (LDL) can penetrate the disturbed endothelium and start oxidation. After modification or oxididation, the LDL engage leukocytes inside the intima of the coronary vessels, creating foamy cells. After the replication and formation of lesions, these specific cells form a fatty streak. These lesions engage smooth muscle cells (SMCs) alongside the fatty streak, leading them to proliferate and produce extracellular matrix consiting mainly of proteoglycans and collagen. The development of the atherosclerotic plaque into fibrous plaque is caused by the accumulation of extracellular matrix produced by the SMCs. Small blood vessels are created when the fibrous plaque is penetrating the coronary vessel’s lumen, potentially leading in a calcification of the plaque. The proteoglycans earlier mentioned are able to connect with the lipoproteins increasing their life span within the intima. This makes then vulnerable to oxidative modification and glycation. The end product of this oxidation (oxidized phospholipids) and glycation of the lipoproteins can spread inflammatory responses. Libby and Lee state that due to the reaction to the hemodynamic, oxidation, inflammation and autoimmune signals, the Matrix metalloproteinases (MMPs) are produced by the endothelial cells modulating the different functions of the vascular cells. These fuctions include proliferation, new vessel formation, activation, migration, cell death, destruction of the extracellular matrix of arteries, geometric remodeling, myocardium and healing. A blockage of blood flow results from the accumulation of atherosclerotic plaque inside the coronary artery, leading to an inbalance between supply and demand of myocardinal oxygen. This inbalance is the root cause of the CHD sysmtoms like heaviness and substernal discomfort, lasting usually for a few minutes, caused normally through distress, heavy meals, the cold or exertion. |
|
Risk factors associated with CHD |
|
In the development of CHD there are risk factors identified being associated with the disease, including smoking, diabetes, obesity, homocystinuria, hyperuricemia and stress. According to the US Department of Health and Human Services smoking affects the atherosclerotic lesion and also stimulates coronary occlusion by creating endothelial denudation and platelet attachment to subintimal layers. This leads to an increase of lipid infiltration and platet-derived growth factor-mediated proliferation of SMCs (PDGF). In this context several studies, including cohort studies and case-control-studies with 20 million people showed the higher death incidence because of CHD in smokers in comparison to nonsmokers with a 70 % higher CHD mortality. Diabetes mellitus or type 2 diabetes, is a risk factor for CHD, due to its connection to hyperlipidemia, a disease defined by increased levels of triglycerides and decreased levels of HDL cholesterol. In patients with type 2 diabetes high levels of total VLDL triglycerides, low levels of HDL cholesterol and high levels of very low-density lipoprotein (VLDL) have been identified as potential risk factors for CHD according to Laasko et al. The Procam Study pointed out a strong connection between hypertension and CHD, but also the association of hypertension with metabolic disorders, that are all known risk factors of this disease, including hyperinsulinemia, dyslipidemia and insulin resistence underlining the link between hypertension and CHD. Obesity is also associated with CHD, as it incorporates the excess aggregation of fat in the adipose tissues which can, in the abdominal visceral, result in atheroscerlotic disease. Homocystinuria is defined as a defect in the metabolism of methionine or an inherited recessive disorder with high levels of urinary homocysteine and homocysteine circulating in such a disorder. According to Mudd et al. patients with homocysteinuria seem to be prone to the early beginnings of cardiovascular diseases. There is evidence by Malinow of the endothelium being resistant to thrombosis as well as the coagulation system being impaired by homocysteine. The definition of Hyperuricemia according to Becker is the excess of serum urate concentration, which is current in the body. Serum uric acid, as a product of the purine metabolism, is the cause of hyperuricemia at concentrations higher than 6.8 mg/dl. Several studies have pointed to a connection between hyperuricemia and the risk of CHD. Stress has also been identified as an important risk factor for cardiovascular diseases as it leads to a decreased insulin sensitivity and to an increase in blood pressure, endothelial dysfunction and hemostasis. In this context psychsocial stress, especially job strain, has also been shown to be a risk factor for CHD. A case-control study by INTERHEART revealed the association between job strain and a higher risk of myocardial infarction (MI) in men than in women. |
| Diagnostics |
|
When diagnosing a CHD, the primary focus is on the medical history by the attending physician with subsequent physical examination. Both invasive (e.g. coronary angiography, coronary angioscopy) and non-invasive procedures (e.g. resting and exercise ECG, echocardiography, MRI) can serve as further diagnostic tools. The prevention of coronary heart disease involves the identification of risk factors while minimizing them. Laboratory diagnostic analysis of parameters and risk markers that are directly related to this disease can make a significant contribution. With the help of ultrasensitive CRPs, chronic inflammation in the vessels can be detected, since they act as an independent marker for early detection when no other risk factors are apparent. The determination of the ultrasensitive CRP supports the estimation of cardiovascular risk in patients with inconspicuous plasma lipid levels, as it reflects the current degree of inflammation in the vessel walls. Increased ultrasensitive CRP is associated with a higher risk of coronary heart disease and peripheral arterial disease. While values < 0.7 mg/l indicate a low risk, values > 5.0 mg/l indicate an acute inflammatory event and values > 1.9 mg/l indicate a high cardiovascular risk. LDL can be oxidized in the extravascular space of the vessel walls. Due to the higher concentrations of antioxidants, it is largely protected from this in the circulation. Oxidized LDL has a high atherogenic potential and can thus trigger low-grade inflammation in the vessel walls. The determination of the value can therefore be used to assess the progression and prognosis of atherosclerotic plaques. Furthermore, oxidized LDL is suspected of promoting the formation of triglycerides and thus increasing fat storage, which in turn increases the formation of oxidized LDL. Physiologically, less than 1% of the LDL circulating in the blood is oxidatively altered, values >235 ng/ml indicate an increased risk. The enzyme lipoprotein-associated phospholipase A2 (Lp-PLA2) is mainly produced by macrophages, T cells, monocytes and mast cells. In advanced atherosclerotic lesions, Lp-PLA2 is particularly expressed and is additionally involved in the oxidative modulation of LDL cholesterol, resulting in oxidized lysophosphatidylcholine and oxidized fatty acids. Consequently, this stimulates the release of adhesion molecules and cytokines, which can trigger further inflammatory processes. Lp-PLA2 is an important predictor of risk because the enzyme is more detectable in unstable plaques that tend to rupture. Laboratory diagnostic tests can be used to determine the activity of Lp-PLA2 in the PLAC® test, which serves as a specific marker for vascular inflammation, since systemic inflammation does not result in elevated levels. The coronary risk is considered increased above a critical activity value of 507 U/l in women and 639 U/l in men. Vascular calcification is a common feature of arteriosclerosis, aging and diabetes mellitus and is also associated with a higher incidence of cardiovascular disease. The matrix γ-carboxyglutamic acid (GLA)-containing protein (MGP) acts as an important local inhibitor of vascular calcification, but only after activation by a vitamin K2-dependent carboxylation reaction. In the presence of a vitamin K2 deficiency, the level of dephosphorylated-uncarboxylated MGP (dp-ucMGP) increases, which promotes the development of artherosclerosis. A lowered vitamin K2 level may not only be due to dietary reasons but may also be caused by the repeated intake of antibiotics, salicylates, vitamin K antagonists as well as alcoholism and liver and chronic gastrointestinal diseases. An increase in dp-ucMGP thus serves as an indication of an insufficient vitamin K2 supply and also acts as a sensitive marker for vascular calcification and cardiovascular disease. The enzyme myeloperoxidase (MPO) is predominantly released by activated granulocytes and is involved in the defence process of microorganisms. In addition, granulocytes can react to contact with cholesterol in the vessel walls with the formation of MPO, which in turn contributes to the formation of foam cells and subsequently promotes the "calcification" of the vessel. Furthermore, MPO has oxidative and pro-inflammatory properties that can lead to an impairment of endothelial function, which is why the enzyme is attributed a central role in the development of coronary heart disease. According to studies, MPO has proven to be a suitable marker in diagnostics (values > 444 ng/ml are considered a risk factor), which indicates acute cardiovascular diseases at an early stage and can be used to estimate the prognosis as well as to identify patients at risk in prevention. Atherosclerotic plaques of the vessel wall with an increased risk of complications have large amounts of inflammatory cells (neutrophils, macrophages) which secrete the heterodimeric protein calprotectin (S100A8/A9), which acts as an alarmin. For this reason, patients with arteriosclerosis are found to have significantly increased serum concentrations of calprotectin on average. Calprotectin serves as an active mediator in the pathogenesis of atherosclerotic lesions, as the binding of the molecule to vascular endothelial cells induces the formation of proinflammatory cytokines and the expression of adhesion molecules, which in turn leads to the promotion of inflammatory and thrombogenic processes in the vessels. Significantly increased levels of serum calprotection are also found in patient groups with myocardial infarction, stroke and thrombosis, since atherosclerotic processes are strong risk factors for cardiovascular disease. In addition, other parameters in associated profiles as well as a micronutrient status of the patient can be collected to determine the cardiovascular risk. |
|
Lifestyle recommendations |
|
In the therapy of CHD, the focus is on alleviating symptoms and positively influencing the course of the disease. The main focus is on lifestyle changes, control of risk factors, medication and measures to improve blood flow in the heart vessels. In order to counteract the progression of atherosclerosis and to prevent the risk of serious complications such as heart attack, cardiac insufficiency and cardiac arrythmia, it is important to eleminate the risk factors of CHD as far as possible. The American Heart Association has established 7 basic rules to prevent cardiovascular disease ("Life's Simply 7"), including: 1. be physically active |
| Relevant micronutrients |
|
An important point in the prevention of CHD is to maintain a healthy weight with the desire for sweets and appetite to weaken. Psyllium (psyllium husk) is a highly swelling fiber that can also be used therapeutically to support weight control measures by counteracting rapidly resurging hunger and appetite. Dietary fibre begins to swell in the stomach, increasing the volume of the chyme. The result is a long-lasting satiation effect that delays the onset of a renewed feeling of hunger. The modulated insulin release also leads to lower appetite and hunger signals at metabolic level. The amino acids 5-hydroxytryptophan, L-tryptophan and L-phenylalanine also reduce the feeling of hunger and L-glutamine reduces the desire for carbohydrates. In the meantime, epidemiological studies and meta-analyses have proven that omega-3 fatty acids play an important role in maintaining the function of the cardiovascular system. Large-scale clinical studies show a significant reduction in the overall mortality rate as well as in mortality from cardiovascular indices and the number of sudden deaths. In addition, alpha-linolenic acid helps to control total cholesterol and LDL levels and reduce atherogenic plaque formation and vascular inflammation. This can reduce the risk of cardiovascular disease by 40 - 60%. The omega-3 fatty acids EPA and DHA also have antihypertensive effects. They can prevent an increase in blood pressure, but also reduce existing high blood pressure. EPA and DHA have antiaggregatory and vasodilatory effects on the endothelial cells of the vessels and can reduce triglyceride levels. In this way they contribute significantly to protection against cardiovascular diseases. They also inhibit the omega-6 metabolism and use the conversion enzymes to build up "good" anti-inflammatory eicosanoids. This reduces the formation of the undesirable vasoconstrictive, proaggregatory and pro-inflammatory eicosanoids from arachidonic acid, which explains the therapeutic effect of omega-3 fatty acids in inflammatory diseases and in cardiovascular prophylaxis. Another important component is the maintenance of a healthy cholesterol level. Niacin has long been used for intervention in hypercholesterolaemia. Substitution with niacin effectively reduces plasma concentrations of VLDL and LDL while increasing HDL levels. Proanthocyanidins (OPC) also appear to have a direct influence on the lipid profile in hypercholesterolaemia. In clinical trials, an intake of 100 mg grape seed extract over 2 months significantly reduced LDL levels in patients with elevated levels. In addition, proanthocyanidins (OPC) increase the oxidation resistance of LDL cholesterol to free radicals Keeping blood pressure low and thus protecting the endothelial cells is an important factor in the prevention of CHD. Secondary plant compounds, such as oligomeric proanthocyanidins (OPC), improve endothelial functions by increasing the synthesis of the gaseous neurotransmitter NO (nitric oxide). NO has a key function in the regulation of vascular tone. It induces muscle relaxation at the receptors of the vascular muscles, resulting in vasodilation. Grape seeds and the pine bark extract Pycnogenol® are particularly rich in OPC. In addition, OPC prevents arteriosclerosis-promoting events in the early stages by preventing oxidative vascular damage. Due to its anti-edematous, anti-inflammatory and antioxidant properties, OPC is also used for the therapeutic treatment of connective tissue weaknesses and as an adjunct therapy in the early stages of venous diseases. OPC increases the capillary blood flow and normalizes the disturbed vascular permeability. It brings the overstretched veins back to their normal average and helps to reduce fluid accumulation in the tissue. In addition, OPC can protect the fine vascular walls and the surrounding connective tissue from age-related oxidative processes. In connection with normal blood levels and the management of diabetes mellitus, the trace elements selenium and chromium have proven insulin mimetic properties. Their activities include the stimulation of glucose uptake, the regulation of glycolysis and the synthesis of fatty acids. As an underlying mechanism, increased phosphorylation of individual key proteins has been described for selenium, whereby selenium intervenes in the insulin signal cascade in a controlling manner. Trivalent chromium appears to have a regulating effect on glucose utilization via cholesterol homeostasis in the cell membranes. The substitution of zinc can normalize a lowered zinc level in diabetics, lead to improved glycemic control and protect against diabetes-induced cardiomyopathies. Blueberry extract has a significant effect on both blood sugar levels and C-reactive protein levels, an indicator of inflammatory processes. Supplementation with a standardized blueberry extract leads to a lower blood sugar level in the fasting state. Abstaining from cigarettes is important to avoid oxidative damage. If it is not possible to give up smoking, sufficiently high antioxidant levels should be achieved to avoid damage caused by the additional oxidative stress. Apart from use in smokers, epidemiological studies have confirmed the link between insufficient antioxidant supply and the occurrence of arteriosclerotic changes. Clear results are available, especially for the vitamin C, vitamin E and beta-carotene supply. These antioxidative systems reduce the oxidation of LDL cholesterol to toxic ox-LDL, prevent lipid peroxidation and membrane changes and appear to counteract arteriosclerotic events by reducing inflammation-promoting cytokines. Other orthomolecular measures for the prevention and treatment of coronary heart disease include controlling homocysteine levels, increasing vitamin D levels, strengthening the heart muscles, improving cardiac performance, reducing the side effects of statins and reducing the risk of thrombosis. An elevated homocysteine level is considered an independent risk factor for cardiovascular disease and additionally increases the risk of arteriosclerotic changes. Vitamin B6, vitamin B12 and folic acid contribute to the normalization of homocysteine metabolism and reduce the progression of a secondary disease. Vitamin D3 has a regulating effect on myocardial calcium homeostasis, on the performance of the heart muscle and on blood pressure. Various studies document an inverse correlation between vitamin D3 levels and cardiovascular mortality. In a large-scale cross-sectional study, a vitamin D deficit compared to good status (calcidiol greater or equal 75 nmol/l) was associated with a 2.8-fold increased risk of death from heart failure and a 5-fold increased risk of sudden cardiac death. Coenzyme Q10 is essential for the energy metabolism of the heart muscle. In cardiological diseases such as heart failure and ischemic heart disease, Q10 levels in the heart muscle are significantly lowered. This energetic depletion of the tissue can be counteracted by regular daily substitution with 60 – 500 mg Q10. In general, coenzyme Q10 is recommended as an adjuvant for chronic heart diseases. Clinical studies have shown that 60 – 75% of patients treated with coenzyme Q10 experienced a significant improvement in performance. After a myocardial infarction, Q10 substitution showed a significant reduction in reactive radicals, thus reducing the risk of further atherothromboses. A significant increase in life expectancy was observed in patients with heart failure. In addition, in clinical studies both systolic and diastolic blood pressure was significantly reduced by Q10 substitution. The coenzyme Q10 status is closely linked to the side effects of cholesterol-lowering statins (CSE inhibitors). The muscle weakness that often occurs as a side effect of statin therapy is attributed to the intervention of CSE inhibitors in the biosynthesis of mevalonic acid. This not only interrupts the build-up of cholesterol, but also the self-synthesis of coenzyme Q10. Tomato extract shows a strong antithrombotic effect based on the stabilization of platelet form by inhibition of thrombin-induced aggregation and inhibition of glycoprotein 2b/3a. In addition, tomato extract contributes to an efficient reduction of oxidative processes. Results from in vitro and animal model studies attest Cannabidiol (CBD) a variety of cardioprotective effects. CBD not only vasodilated cells of human mesenteric arteries, but also reduced the extent of heart attacks in animal experiments. At the same time, a reduction of myocardial dysfunction and a weakened inflammatory response were observed. In this context a recent meta-analysis of 25 in vivo studies evaluated the effects of CBD on blood pressure, heart rate and blood flow. It concluded that CBD affects the cardiovascular system especially under stress: The CBD intervention reduced both the increase in blood pressure and the increase in heart rate statistically significant. |